(also known as gynecomastia surgery)
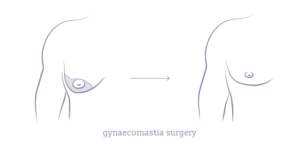
Gynaecomastia surgery, often referred to as male breast reduction, is a surgical solution designed to reduce enlarged breast tissue caused by gynaecomastia. The surgery involves the removal of excess fat, glandular tissue, and sometimes skin to achieve a flatter, more traditionally masculine chest contour.
Gynaecomastia can affect men at any age due to hormonal imbalances, weight gain, or genetics. This corrective surgery uses liposuction, excisions or a combination of both techniques to achieve a more aesthetic and comfortable appearance for patients.
Surgical Warning: Any surgical or invasive procedure carries risks. Before proceeding you should seek a second opinion from an appropriately qualified health practitioner.
Read more on the Risks of Surgery
What is gynaecomastia?
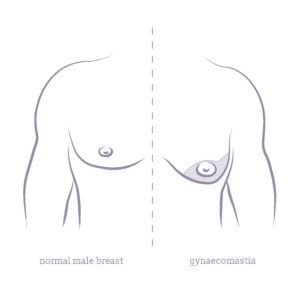
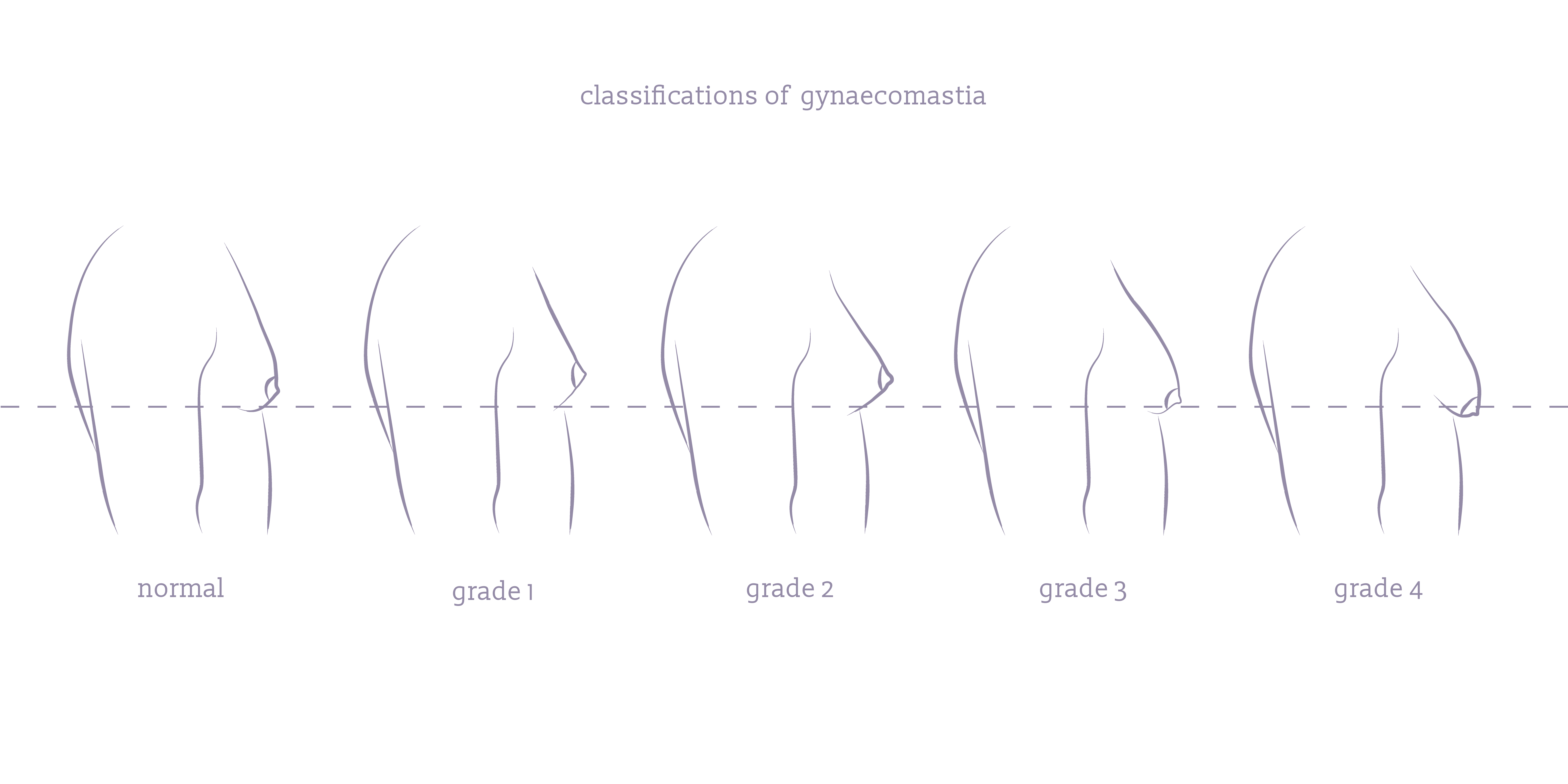
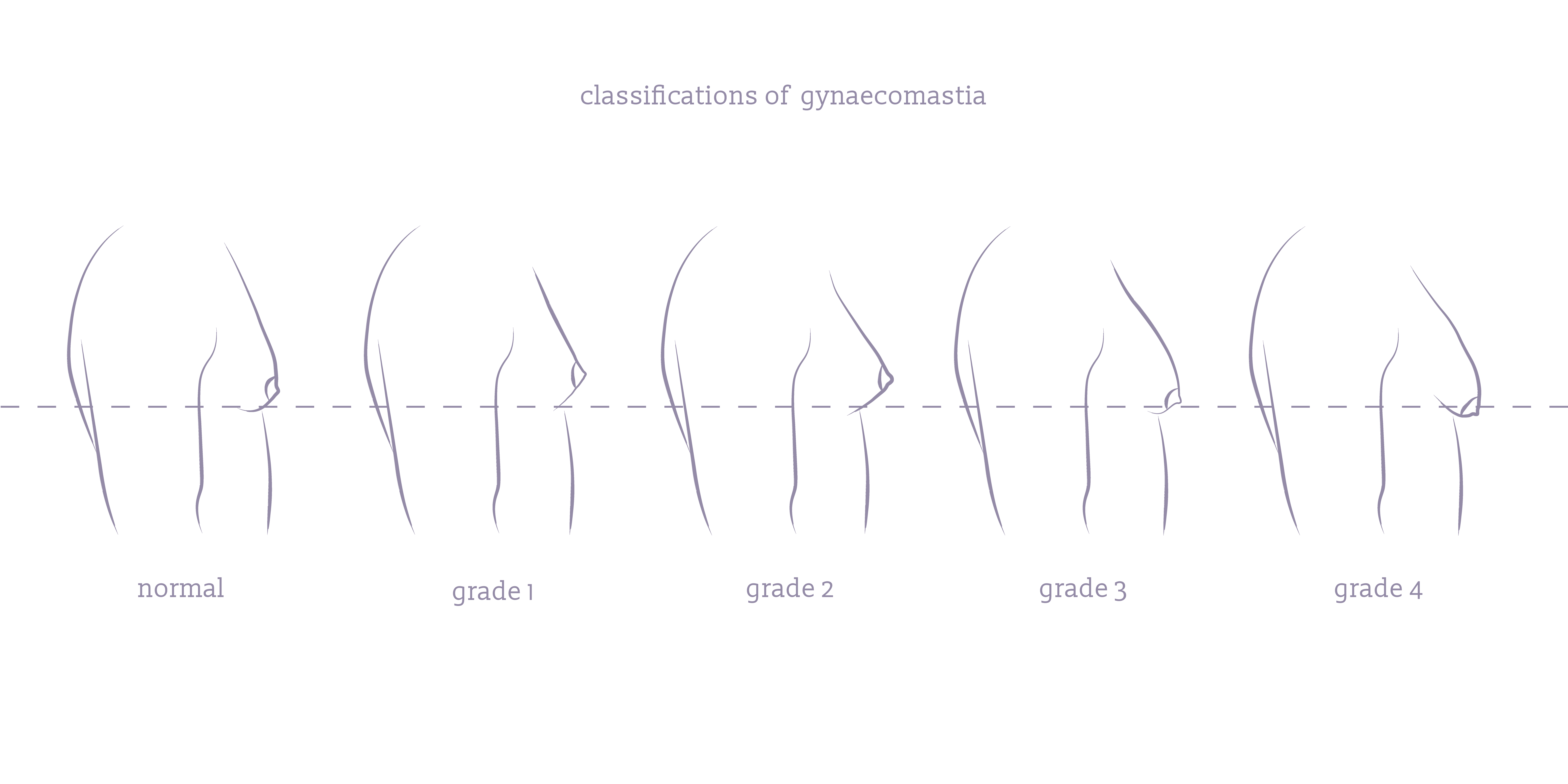
Gynaecomastia, often casually referred to as “man boobs” or “gyno”, is characterised by the enlargement of breast tissue in males. This condition of enlarged male breasts can vary in severity from a small amount of extra tissue around the nipples (grade 1) to more significant and noticeable breast enlargement (grade 4). Although gynecomastia itself is not medically dangerous, it can sometimes be a symptom of underlying health issues that may require attention.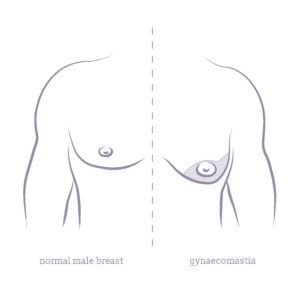
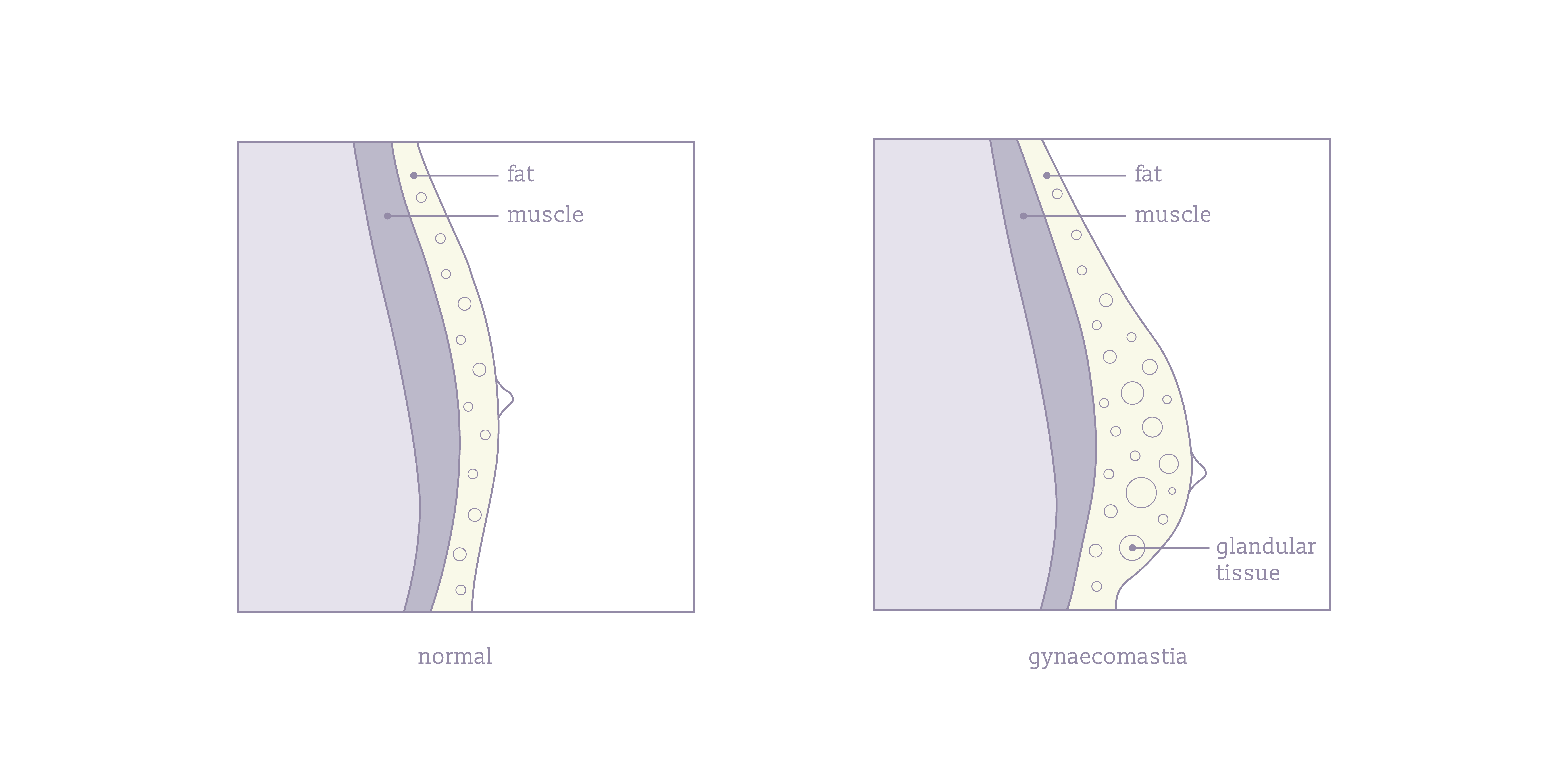
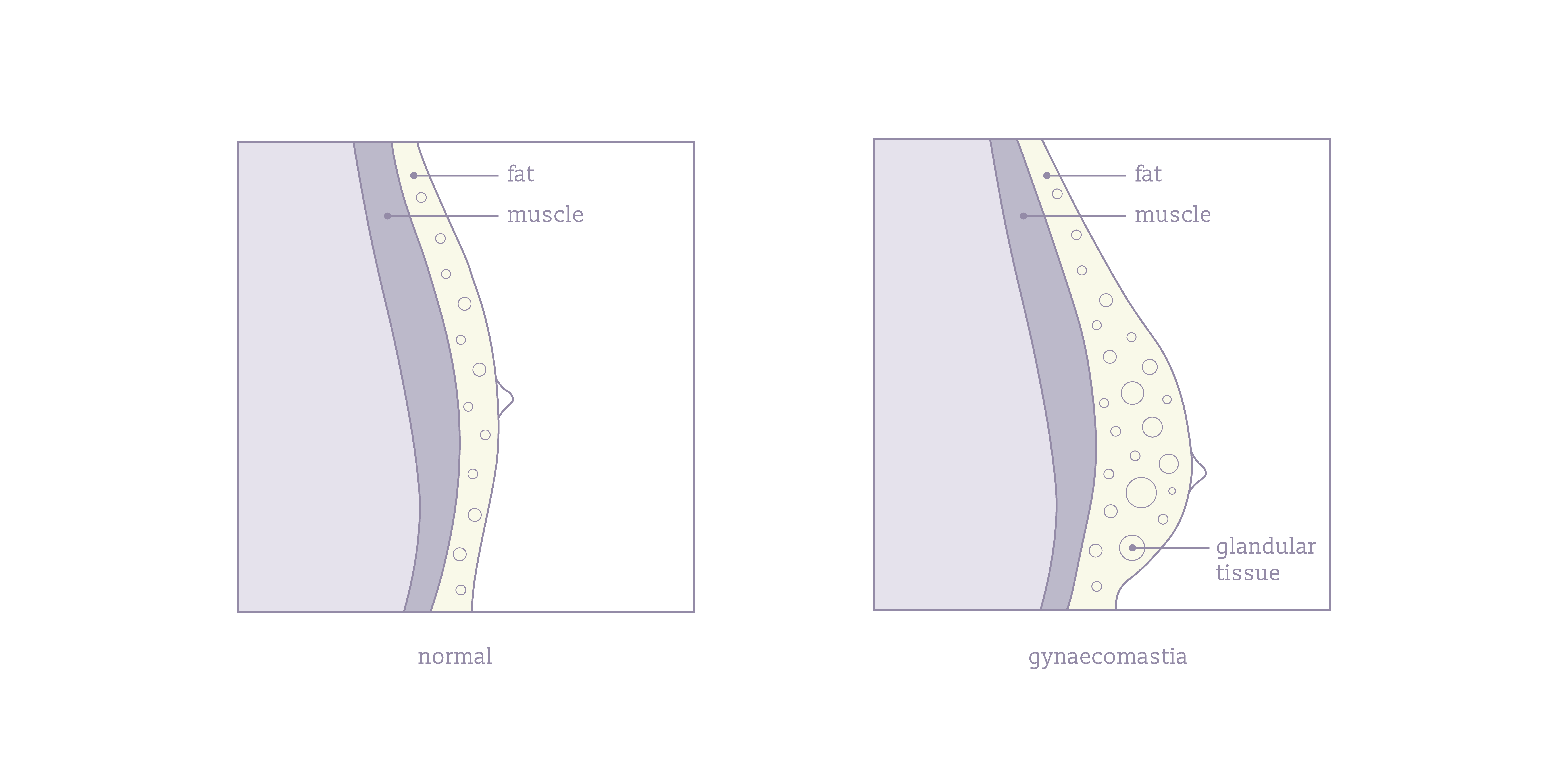
Gynaecomastia can affect one breast (unilateral), however bilateral gynaecomastia is more common studies have found. Glandular tissue in the male breast is responsible for the development of gynaecomastia as it grows due to imbalances in hormones. This tissue is firm and fibrous, contributing to breast enlargement that differs from pseudogynecomastia, where the enlargement is due to excess fatty tissue, which is softer and more widespread across the chest area.
Understanding the types and severities of gynaecomastia is crucial as it influences the approach to treatment and the surgical techniques employed, such as liposuction for fatty tissue or excision for glandular tissue removal. Individuals can develop a mix of these tissues, with optimal treatment often involving a combination of surgical techniques tailored to the specific tissue composition present.
Gynaecomastia Causes
Gynaecomastia is primarily caused by an imbalance between the hormones testosterone and estrogen. When estrogen levels are relatively high compared to testosterone, it can lead to the development of breast tissue. Several factors can contribute to this hormonal imbalance:
Natural life stages
Puberty and aging can shift hormone levels, increasing the risk of developing gynaecomastia. In some cases breast tissue shrinks naturally after puberty typically due to hormonal rebalancing. This is known as asymptomatic gynecomastia, however in most cases the breasts remain enlarged.
Medication
Certain drugs, including anti-androgens for prostate cancer, anabolic steroids, HIV medications, and some treatments for heart conditions, can promote the growth of male breast tissue.
Substance use
Alcohol, amphetamines, marijuana, and heroin are known to affect hormone levels. Additionally, some herbal compounds found in over-the-counter products like shampoos or lotions can subtly alter hormone balances.
Health conditions
Disorders that affect hormonal balance, such as hypogonadism, thyroid problems, and kidney or liver disease, can lead to gynaecomastia. Tumors involving the testes, adrenal glands, or pituitary gland can also alter hormone levels.
Gynaecomastia Symptoms
The symptoms of gynaecomastia can vary depending on the extent of breast tissue enlargement. Common signs include:
- Increased size of the chest, which can be unilateral or bilateral.
- Tender breast areas that are sensitive to touch.
- Breast tissue is typically soft and can be moved slightly under the skin.
- Nipple discharge from one or both nipples in rare cases.
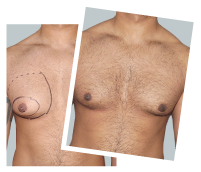
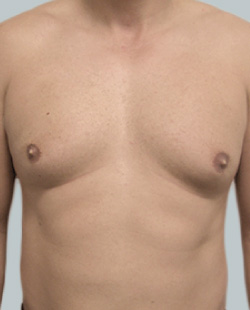
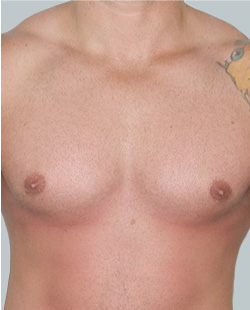
Before 
After 
Performed By: Dr Ashley Granot (M0001026218) MBBS, FFMACCS (Med), FACP, FACNEM, ABBRM, MA5M Cosmetic Doctor, Melbourne
Is gynaecomastia surgery right for me?
Deciding if gynecomastia surgery is right for you involves evaluating various factors that affect both your physical health and emotional well-being. Gynecomastia surgery is the definitive treatment for persistent gynaecomastia, especially when other non-surgical treatments have failed to yield results. The decision ultimately hinges on individual health, cosmetic goals, and the presence of fatty or glandular breast tissue.
Benefits of gynaecomastia surgery
There are many benefits and reasons for gynecomastia surgery that should be considered. When the excess breast tissue is removed it can achieve the following:
- A more masculine and contoured male chest through breast size reduction.
- Effective removal of excess tissue that lifestyle changes could not eliminate, especially when gynaecomastia is primarily glandular.
- Discomfort and pain relief associated to enlarged breasts and skin irritations.
- Enhanced confidence that enlarged male breasts would otherwise detract from.
- Increased physical activity as men find engaging in physical activity more comfortable and enjoyable after gynecomastia surgery.
- Minimal scarring with advanced surgical techniques and incisions made in less visible areas around the areola and under armpit.
- Quick recovery with modern surgical methods and pose-operative care protocols.
- Is the definitive male breast reduction method that is permanent when paired with healthy lifestyle choices.
Ideal candidates for gynaecomastia surgery
- Men that have experienced persistent gynecomastia that has not resolved naturally over time or through other medical treatments.
- Men that are bothered by their gynecomastia and desire male breast reduction surgery.
- Individuals with a stable weight as weight fluctuations can affect surgery results.
- Non-smokers or those who can quit smoking well before and after surgery as smoking effects the healing process.
- Patients with realistic expectations of gynecomastia surgery and what it can can achieve.
- Free from any medical conditions and of good health.
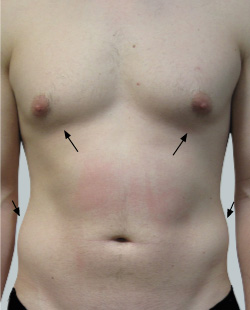
Before 
After 
Performed By: Dr Ashley Granot (M0001026218) MBBS, FFMACCS (Med), FACP, FACNEM, ABBRM, MA5M Cosmetic Doctor, Melbourne
Gynaecomastia surgery overview:
- general anaesthetic
- small incisions to remove excess breast tissue
- surgical methods of liposuction and/or excisions
- same-day discharge from hospital
What does gynaecomastia surgery involve?
Male breast reduction surgery typically requires general anaesthesia, although local anaesthetic may be used in less severe cases. A plastic surgeon will make small incisions that differ in type and location according to the extent of the gynaecomastia and the surgical method being used. The incisions are often around the nipple or within the natural creases of the chest.
If the gynecomastia is characterised mainly by excess fatty tissue with good skin elasticity, liposuction is employed. A cannula is inserted through the incisions to vacuum out the fat.
However, for glandular tissue removal or when significant loose skin needs addressing, skin excision is required for tightening. This may also involve the resizing or repositioning of the areola and nipple to achieve a more natural male chest contour.
After the removal of excess breast tissue, the surgeon proceeds to adjust and reshape the remaining tissue to ensure a smooth contour and aesthetically pleasing chest appearance. This is when the repositioning or resizing of the nipple occurs if necessary.
The final step in the procedure involves closing the incisions. This is done using sutures that may either dissolve over time or require removal during a follow-up visit. Incision lines are generally planned to be hidden around the nipple or creases of the chest to minimise visible scarring. Patients may be placed into a compression garment to control swelling.
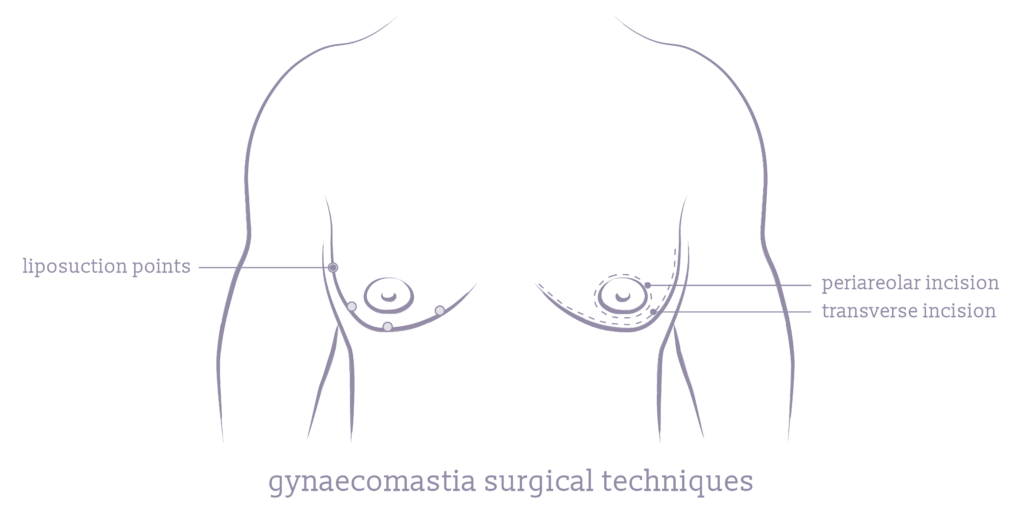
Gynaecomastia surgical techniques
Plastic surgeons select different surgical techniques for gynecomastia plastic surgery based on the specific characteristics and needs of each patient. Factors such as the extent of excess breast tissue, the presence of glandular versus fat tissue, and the patient’s overall body composition and aesthetic goals dictate the most effective approach to achieve optimal results.
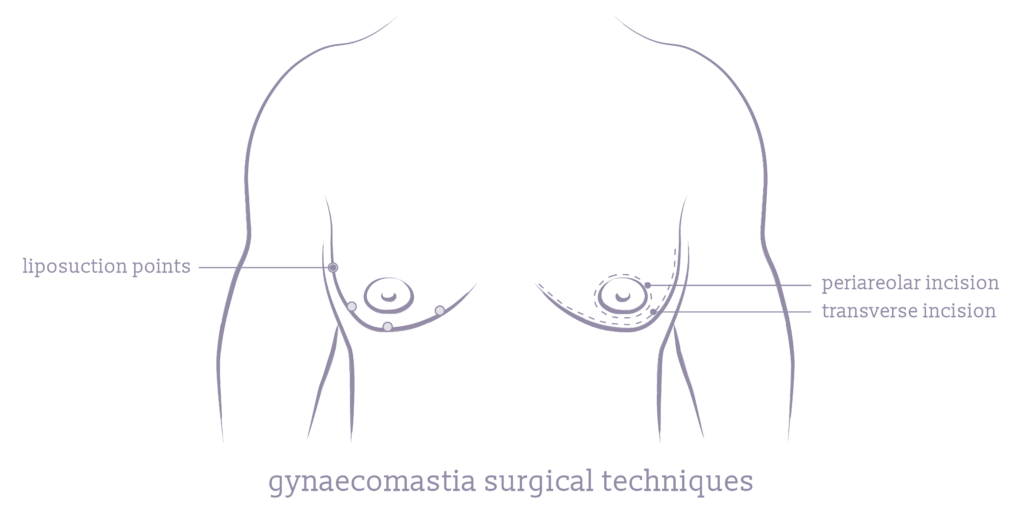
Liposuction
This method is primarily used to remove excess fat and is suitable for patients without significant glandular involvement. Liposuction involves suctioning out fat tissue through small incisions, offering minimal scarring.
Donut Incision
The periareolar incision (donut) technique is used for mild to moderate gynecomastia. It involves making an incision around the areola’s edge, allowing for the removal of glandular tissue directly beneath the nipple. This method effectively reduces breast gland size and is advantageous for its well-concealed scars that blend with the natural contours of the areola.
Transverse Incision
This incision is optimal for severe gynaecomastia, particularly in cases after massive weight loss where there is a significant amount of excess skin. The transverse incision is made horizontally across the lower chest area, often extending from the underarm to the chest. It can be combined with a peri-areolar (donut) incision to enable comprehensive tissue removal and skin tightening. This combination can relocate the nipple, creating a more naturally contoured chest when needed.
Combination of Excision and Liposuction
This approach is effective for cases with both glandular and fatty tissue, providing comprehensive results by addressing all excess tissue types. It combines fat removal via liposuction and glandular breast tissue excision through strategic incisions, suited for a wide range of gynecomastia cases.
What happens directly after gynaecomastia surgery?
Immediately after gynecomastia surgery, most patients are monitored in the recovery area as anesthesia wears off. During this time, it’s common to experience mild discomfort, which can be effectively managed with prescribed medications. A compression garment is applied to help reduce swelling.
Before you are discharged, you will be given specific instructions on how to care for yourself in recovery. These include how to care for your incisions, methods for pain relief, and signs of potential complications to watch for. It is essential that a responsible adult is available to drive you home and assist you during the first night after your procedure, ensuring your safety and comfort as you begin your recovery at home.
Before gynaecomastia surgery
Before your male breast reduction surgery, an initial consultation followed by a detailed diagnostic process to confirm the presence and type of gynaecomastia will occur. Patients receive instructions on how to prepare for the surgery to optimise outcomes and reduce the risk of complications. Understanding these preparatory steps helps patients feel more confident and informed about their surgical journey.
Gynaecomastia Consultation and Diagnosis
The first step in the process is a comprehensive consultation with a specialist plastic surgeon in male breast reduction. During this meeting, the surgeon will evaluate your medical history, conduct a physical examination of the breasts, and discuss your expectations and goals for the surgery. Referrals for diagnostic tests, such as ultrasound or mammography, may be employed to differentiate between fatty and glandular tissue, helping to determine the most effective surgical approach. Importantly, this process ensures whether there are no underlying causes for your gynaecomastia.
This consultation ensures that you are a candidate for gynecomastia surgical correction, the grade of your condition, and the most appropriate surgical option.
How to Prepare for Gynaecomastia Surgery
Preparing for gynaecomastia surgery involves several important steps:
- Complete any requested health screenings or tests to ensure you are fit for surgery.
- Discuss your current medications with your surgeon, as some may need to be adjusted or stopped prior to surgery.
- If you smoke or consume alcohol, you will likely need to stop as these can affect your recovery and surgery results.
- Follow the fasting instructions for the night before and morning of your procedure, as recommended by your surgeon.
- Plan for someone to drive you home after your procedure and help you during the first few days of your recovery.
- Set up a comfortable environment in your house for recovery.
Questions to Ask Your Gynaecomastia Surgeon
It is important to ask these several key questions during your consultation to fully understand the procedure and set realistic expectations:
- What are the expected outcomes of my surgery?
- What surgical technique will be used, and why?
- What can I expect in terms of recovery and potential side effects?
- How are complications handled?
- Can I see before and after photos of your previous patients who had similar conditions?
- What are the costs involved, and is there coverage or financing available?
The consultation is the best place to ask questions and to answer any uncertainties you might have. Asking these questions and others, will provide you with a clearer understanding of what to expect and also help build a trusting relationship with your surgeon.
Gynaecomastia recovery
Key recovery information for male breast reduction surgery:
- Return to work and light activities usually 1-2 weeks.
- Swelling and bruising, significantly reduced around 3 weeks.
- Strenuous exercise avoided until 3-4 weeks or surgeon’s instructions.
- Pain subsides after first week, manageable with pain medication.
Gynaecomastia Recovery Timeline
The recovery timeline for gynecomastia surgery can typically look like the following:
First 24 Hours
Immediate post-operative period under close observation, often with pain management medication.
First Week
Rest with limited activity; wearing of a compression garment begins. Light activities to begin towards the end of the first week.
Second to Third Week
Gradual reduction in swelling and bruising; possible return to work and light daily activities. Swelling and bruising to significantly reduce around 3 weeks.
One Month
Assessment in follow-up visit to check on the surgical site and progress of recovery.
Six Weeks
Most patients can resume their regular exercise routine and more strenuous activities if the surgeon gives the clearance.
Gynaecomastia Post-Operative Care
Effective post-operative care is crucial for achieving the best results and smooth recoveries after gynecomastia surgery. Key aspects include:
- Wearing compression garments as instructed helps reduce swelling and supports the new chest contour.
- Pain is typically manageable with prescribed medications; it’s important to follow the dosage and scheduling recommendations.
- Avoid lifting heavy objects or engaging in high-impact activities during the initial recovery phase to prevent complications.
- Keep surgical sites clean and dry, and follow specific instructions for showering and changing dressings.
- Watch for signs of infection or unusual discharge and report these to your surgeon immediately.
Adhering to these guidelines helps ensure that your recovery from gynecomastia surgery progresses smoothly and without common complications.
Male breast reduction surgery results
Gynecomastia surgery effectively removes excess skin, tissue, and/or fat, offering permanent results for male breast reduction. To maintain and enhance these results, adopting healthy post-surgical lifestyle habits is crucial. Regular exercise, a balanced diet, and maintaining a stable weight are essential to prevent the recurrence of fat deposits.
Additionally, adhering to the surgeon’s care instructions and attending follow-up appointments will ensure the longevity of the surgical outcomes and help manage any potential health issues that could influence breast size.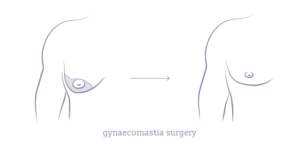
Will there be scars after gynaecomastia surgery?
Scarring is an inevitable part of any surgical procedure, including gynecomastia surgery. However, plastic surgeons typically make efforts to minimise the visibility of scars by placing incisions strategically—often around the areola or within the natural creases of the chest. Over time, these scars usually fade and become less noticeable. Post-operative care, including proper wound care and following specific guidelines on sun exposure and using scar-minimising treatments, can further help reduce the appearance of scars.
Gynaecomastia surgery cost
The cost of gynaecomastia surgery can vary significantly from one patient to another, depending on several key factors. This includes complexity of the specific case and surgical techniques used, the surgeon’s expertise and additional factors like anesthesia fees and facility charges.
Due to these variables, it’s difficult to pinpoint an exact cost without a consultation, but generally, gynecomastia surgery costs start at $8000 to $9500. This price is often less due to rebates and your health fund.
Can I get a medicare rebate for gynaecomastia surgery?
In some cases, a Medicare rebate for gynaecomastia surgery is possible, particularly if the procedure is deemed medically necessary rather than purely cosmetic. To qualify for a rebate, you must have a referral from a general practitioner and the surgery must be performed by a qualified specialist plastic surgeon.
The specific criteria often involve proving that the gynaecomastia is causing significant physical discomfort or psychological distress. Patients are encouraged to discuss their individual circumstances with their surgeon, who can provide documentation to support a Medicare claim. Additionally, if you have private health insurance, it may cover some of the hospital or anesthetist’s fees, depending on your policy.
Find out if you are a candidate for gynecomastia surgery
Me Clinic is a clinic in Australia that offers plastic and cosmetic surgery procedures. We work with highly qualified surgeons, clinicians, and anaesthetists who are experienced in treating a wide range of medical conditions. We support our patients from the initial consultation through to recovery and post-surgery aftercare.
You can contact Me Clinic and book a consultation for a personalised one-on-one in clinic, video or phone chat with a qualified Me Clinic surgeon. Alternatively, use the handy online consultation form for more information.
Our Practioners Who Specialise in Gynecomastia Surgery in Melbourne:
Dr Amir Tadros
MBBS, FRACS(Plast),FRCS(Ed), FESSH (Dip), MD, MBChB, MRCS, BSc (Hons)
Specialist Plastic Surgeon (MED0001375519)
Mr. Amir Tadros is a triple board-certified Specialist Plastic Surgeon with over 25 years of experience, performing thousands of cosmetic and reconstructive surgeries in Australia, the UK, and internationally. His extensive training in world-renowned plastic surgery units and expertise in complex cases ensure patients receive the highest level of surgical precision and care.
Read more
Dr David Ross
MB BS, FRACS(Plast.) FRACS(Plast)
Specialist Plastic Surgeon (MED0001124797)
Dr David Ross is a Specialist Plastic Surgeon with over 27 years of experience in plastic surgery and cosmetic procedures. Dr Ross also has public hospital appointments in supervisor roles, overseeing the training of 25 Specialist Plastic Surgeons during that time. Dr David Ross has published many articles on reconstructive and cosmetic plastic surgery while educating general practitioners.
Read more
Are gynaecomastia surgery results permanent?
Results are typically permanent, but factors like hormonal fluctuations or significant weight changes can affect them. Maintain a healthy lifestyle to preserve results.
How can I minimise scarring from gynaecomastia surgery?
Choose a skilled surgeon for less visible incisions and follow post-surgery instructions, including the use of recommended scar treatment products like silicone gel sheets. Keep the scars shielded from the sun.
What are the risks and possible complications with gynecomastia surgery?
Gynecomastia surgery, like any surgical procedure, carries risks and potential complications. Complications include changes in nipple sensation or the development of inverted nipples, loss of nipple skin, contour irregularities and loose breast skin if the skin does not adequately conform to the new chest contour post-surgery.
In rare cases, complications such as a blood clot or deep vein thrombosis can develop. It’s important to monitor any unusual changes in the breast tissue post-operatively. Patients should discuss all potential risks with their surgeon to fully understand the scope of possible surgical outcomes and ensure that appropriate measures are taken to minimise complications.
Is there a non-surgical treatment for gynaecomastia?
Hormone therapy may address hormonal imbalances, and lifestyle changes can help reduce fatty gynecomastia. True glandular gynecomastia usually requires surgical intervention.
Will gynaecomastia disappear if I lose weight?
Weight loss may reduce fatty gynecomastia but won’t affect glandular tissue, which typically requires surgical correction.
Are there different types of gynaecomastia?
Gynecomastia can involve fatty tissue (pseudogynecomastia) or glandular tissue, the latter often linked to hormonal imbalances. Both types may be present in some cases.
How common is gynaecomastia in men?
Gynecomastia is quite common, affecting up to 70% of boys during puberty in a mild or temporary form and about 65% of older men, reflecting natural hormonal changes.
Is gynaecomastia surgery painful?
You won’t feel pain during the procedure due to anesthesia. Patients report that post-operative discomfort is typically mild to moderate and well-managed with medication.
When should I consider surgery for my gynaecomastia?
Any male with enlarged breasts who is in good health, a non-smoker with realistic goals for the procedure is a good candidate for gynaecomastia correction or male breast reduction.
Is gynaecomastia dangerous if left untreated?
Gynaecomastia itself is not medically dangerous and can not lead to breast cancer. It can be a symptom of underlying health issues that may need investigation. While not treating gynecomastia doesn’t lead to physical health risks, it can cause emotional or psychological distress.
What is the recovery time for gynaecomastia surgery?
Recovery usually takes one week for light activities, with complete recovery spanning several weeks to months.
How is gynaecomastia diagnosed?
Diagnosis involves physical exams, medical history review, and possibly imaging tests or blood tests to differentiate tissue types and check for hormonal imbalances.
When can I start exercising after gynaecomastia surgery?
Light activities like walking can resume a few days post-surgery, but avoid strenuous exercise for 3 to 4 weeks or until your surgeon gives you the clearance to do so to ensure proper healing.
How do I prepare for gynecomastia surgery?
Preparing for male breast reduction surgery involves stopping certain medications, avoid smoking and alcohol, arrange transportation for procedure day, and prepare a recovery area at home.
What happens during gynecomastia surgery?
Gynecomastia surgery involves anesthesia, making incisions around the areola or armpits, and removing problematic tissue via liposuction or excision, depending on the gynecomastia type.
Can I get gynaecomastia on one chest and not the other?
Yes, gynecomastia can occur unilaterally (in one breast) or bilaterally (in both breasts). Unilateral gynecomastia is less common, but leads to an asymmetric appearance of the chest.
Why is gynecomastia common in bodybuilders?
Bodybuilders often experience gynecomastia due to anabolic steroids or supplements that alter hormone levels, increasing estrogen relative to testosterone.